Do you often fall asleep in the middle of activities? You may be suffering from narcolepsy. Read about narcolepsy facts and statistics to learn more.
Narcolepsyis a type of neurologicalsleep disorderwhereby the brain cannot regulate sleep-wake cycles. People suffering from narcolepsy are known to fall asleep at inappropriate times, like while having a conversation, driving or eating a meal. Recent clinical and epidemiological studies provide a better understanding of narcolepsy with the most up-to-datenarcolepsy facts and statistics.
How Common is Narcolepsy?
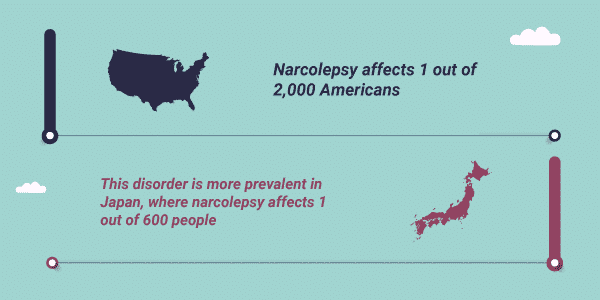
The prevalence of a disease is a measure of how common that disease is in a given population. Narcolepsy affects1 out of 2,000Americansand3 millionpeopleworldwide. Interestingly, this disorder is more prevalent in Japan, where roughly1 out of 600people suffer from narcolepsy.
The onset of narcolepsy typically occurs between the ages of10–30and impactsmen and womenequally.
Narcolepsy is thought to be caused by bothgeneticandenvironmental factorsrelated to the immune system, though its specific cause is unknown. Some of these factors differ based on thetype of narcolepsy.
New Year, New Beginnings.
Whether you are struggling with addiction, mental health or both, our expert team is here to guide you every step of the way. Don’t wait— reach out today to take the first step toward taking control of your life.
Types of Narcolepsy
Currently, there are three different types of narcolepsy. The two most common forms of the condition differ based on a condition known ascataplexy. A third type, known as secondary narcolepsy, can develop after a brain injury.
- Type 1:Type 1 narcolepsyis formerly known as narcolepsy with cataplexy.Cataplexyis defined as a sudden uncontrollable paralysis in the muscles of the face, arms, legs or core. It is usually brought on by a change in emotional state, such as laughing. Cataplexy is attributed to low levels of a brain hormone known ashypocretin. The main role of hypocretin is to regulate rapid eye movement (REM) sleep, which is a critical component of healthy sleep.
- Type 2:Type 2 narcolepsyis similar to type 1 except that no cataplexy is present and hypocretin levels arenormal.Symptomssuch as excessive tiredness, hallucinations while falling asleep or waking up, sleep paralysis and vivid dreams are common in both type 1 and type 2 narcolepsy.
- Secondary Narcolepsy:Secondary narcolepsymay develop after an injury to the hypothalamus, a region in the brain responsible for sleep regulation.
Narcolepsy Misdiagnosis
Astudy from 2016found that of patients with a confirmed narcolepsy diagnosis, almost 50% weremisdiagnosed. This study demonstrates that there is a desperate need to improve diagnostic criteria for the disorder. Amisdiagnosisof narcolepsy has long-term implications, such as limited employment options, unnecessary use of prescriptions, insurance-related issues and inability to drive. To accurately diagnose narcolepsy, medical professionals must take a detailed medical history, conduct a physical examination and recommend a sleep study.
Various sleep study tests are used in the diagnosis of narcolepsy. The most common tests include:
- Polysomnogram: Apolysomnogramis performed overnight at a sleep center. These test monitors brain activity to determine how quickly patients fall asleep or enter REM sleep.
- Multiple Sleep Latency Test:Thistesttakes place in the daytime after a full night of sleep and is used to determine how quickly a patient falls asleep, even after adequate rest.
- Spinal Tap: A spinal tap may be performed to determine hypocretin levels in the spinal fluid.
Narcolepsy and Related Conditions
Narcolepsy has a specific set of signs and symptoms, causes, diagnosis and treatment, some of which overlap with related conditions. Some of these associated conditions include:
- Depression: Since the 1970s, it has been known that narcolepsy is associated with anincreased risk of depression, potentially through a mechanism involving hypocretin.
- Anxiety: Astudypublished in 2010 found that 35% of narcoleptics met diagnostic criteria for ananxiety disorder, regardless of age or sex.
- Sleep Paralysis:Sleep paralysisis often a symptom of narcolepsy. Narcoleptics may experience sleep paralysis and hallucinations while falling asleep or waking up.
- Post-Traumatic Stress Disorder(PTSD): Otherwise known asPTSD, there arepotential linksinvolving REM sleep cycles between this disorder and narcolepsy
- Substance and Alcohol Use: There has been at least onecase studywhereby heavy alcohol use was thought to bring about the development of narcolepsy; however, there are currentlynot enough studiesavailable to determine causal linkages betweensubstance use and narcolepsy.

Narcolepsy and Driving
Driving with narcolepsycan pose a serious safety risk to oneself and others if the disorder is not properly managed. TheNexus Narcolepsy Registrydetermined that while 94% of narcoleptics used their prescribed narcolepsy medication, almost 35% were involved in at least onemotor vehicle accident. In the United States,different stateshave different rules about driving with narcolepsy.
Narcolepsy Research and Prognosis
Currently, there isno curefor narcolepsy, nor do symptoms of the condition dissipate over time. However, scientists and medical professionals are actively conductingresearch and sleep studiesto better understand this disorder.
Arecent studyprofiled blood from narcoleptic patients and found an elevated immune response in these individuals.Another studyinvolving rodents suggested that certain components of the immune system were attacking proteins necessary for hypocretin response, leading to narcoleptic symptoms in these mice. This data further supports the crucial role of the immune system in narcolepsy.
According toHarvard Health, theprognosis for narcolepsyis bleak if the disease is not managed correctly, namely because narcoleptics are at amuch higher riskfor work-related injuries or motor vehicle accidents than members of the general population.
Statistics on Narcolepsy Treatment
It is estimated that the narcolepsy is probably underdiagnosed, with only 25% of people currently seeking treatment. This gap in treatment may be attributed to people who experience mild narcolepsy symptoms and do not seek medical care. Nevertheless, there are numeroustreatments for narcolepsydepending on the symptoms and type of narcolepsy.
Medical professionals use the current standard of care as a guideline for treating all patients diagnosed with narcolepsy:
- Both type 1 and type 2 narcolepsy can be treated with stimulants and scheduled naps to prevent daytime sleepiness. Stimulants likeamphetamine saltsare most effective at doses between 5-60 milligrams.
- Type 1 narcolepsy or sleep paralysis can be treated effectively withantidepressantsat varying doses.
- Symptoms of type 1 narcolepsy can be addressed with a neurotransmitter calledgamma hydroxybutyrate, which is most effective at split doses (one day and one nighttime dose) between 4.5–9 grams.
It is likely that, in the near future, treatments for narcolepsy will target specific components of the immune system. Until then, thebest treatments for narcolepsyare the current standards of care aimed at reducing symptoms and improving the individual’s safety.
If you or a loved one are struggling withco-occurring addiction and narcolepsy, The Recovery Village can help. You can receive comprehensive treatment for these co-occurring disorders from one of thefacilities located throughout the country. To learn more about treatment programs,call The Recovery Villageto speak with a representative today.




